Breast Cancer Brain Mets Stories
The journey of a patient diagnosed with breast cancer brain metastases (BCBM) is uniquely challenging, both physically and emotionally. BCBM occurs when breast cancer cells spread to the brain, leading to the formation of metastatic tumors. This condition can significantly impact a patient’s quality of life, cognitive function, and overall prognosis. Understanding the personal stories and experiences of those who have faced BCBM can provide valuable insights into the complexities of this condition and the importance of comprehensive care and support.
Understanding Breast Cancer Brain Metastases
Breast cancer is one of the most common cancers among women worldwide. While significant advances have been made in the treatment of breast cancer, the development of brain metastases remains a critical issue. Brain metastases are more common in certain subtypes of breast cancer, such as HER2-positive and triple-negative breast cancer. The symptoms of BCBM can vary widely, including headaches, confusion, seizures, and difficulties with speech and movement, depending on the location and size of the metastatic tumors in the brain.
Personal Stories of Resilience
The Story of Sarah: Diagnosed with stage II breast cancer at the age of 35, Sarah underwent a mastectomy, chemotherapy, and radiation. Two years later, she began experiencing persistent headaches and blurred vision. An MRI revealed several metastatic tumors in her brain. Despite the devastating news, Sarah opted for aggressive treatment, including whole-brain radiation therapy and targeted therapy. Her story highlights the importance of vigilance and the role of advanced diagnostic techniques in early detection and management of BCBM.
The Journey of Maria: Maria, a mother of two, was diagnosed with HER2-positive breast cancer. After initial treatment, she was considered to be in remission. However, several months later, she started experiencing seizures, leading to the discovery of brain metastases. Maria’s case underscores the need for ongoing surveillance and the potential for brain metastases even after successful initial treatment of the primary breast cancer.
Living with BCBM: The Experience of Emily: Emily’s diagnosis of triple-negative breast cancer was followed by a prolonged and challenging treatment regimen. The discovery of brain metastases a year later added a new layer of complexity to her care. Her story emphasizes the psychological impact of living with a metastatic disease and the crucial role of palliative care, cognitive rehabilitation, and support networks in maintaining quality of life.
Advances in Treatment and Management
The management of BCBM has evolved significantly, with a focus on multidisciplinary care that includes surgery, radiation therapy, chemotherapy, targeted therapy, and immunotherapy. The choice of treatment depends on several factors, including the number and location of brain metastases, the subtype of breast cancer, the patient’s overall health, and previous treatments.
- Surgical Interventions: Surgery may be considered for accessible, solitary brain metastases, especially if they are causing significant symptoms.
- Radiation Therapy: Whole-brain radiation therapy (WBRT) and stereotactic radiosurgery (SRS) are used to control the growth of tumors within the brain.
- Systemic Therapies: Chemotherapy, targeted therapy, and immunotherapy can be effective in managing BCBM, particularly in patients with HER2-positive or hormone receptor-positive breast cancer.
Future Directions and Hope
Despite the challenges posed by BCBM, there is a growing sense of hope and optimism. Ongoing research into the biology of brain metastases, the development of new therapeutic agents, and the exploration of novel approaches such as immunotherapy and personalized medicine hold promise for improving outcomes.
For patients and their families facing BCBM, connecting with others who have shared similar experiences can be incredibly empowering. Support groups, both online and in-person, provide a platform for sharing stories, seeking advice, and finding comfort in a community that understands the unique trials and triumphs of living with breast cancer brain metastases.
Frequently Asked Questions
What are the signs and symptoms of breast cancer brain metastases?
+The signs and symptoms of BCBM can include headaches, confusion, difficulty with speech, seizures, weakness or numbness in the face, arm, or leg, and difficulties with balance and coordination. These symptoms can vary depending on the location and size of the metastatic tumors in the brain.
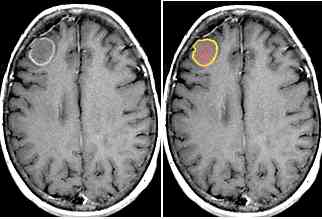
How is breast cancer brain metastases diagnosed?
+Diagnosis of BCBM typically involves a combination of clinical evaluation, imaging studies such as MRI or CT scans of the brain, and sometimes, a biopsy of the brain tissue. These diagnostic tools help in identifying the metastatic tumors and assessing their impact on brain function.
What are the treatment options for breast cancer brain metastases?
+Treatment options for BCBM include surgery, radiation therapy (such as whole-brain radiation therapy or stereotactic radiosurgery), chemotherapy, targeted therapy, and immunotherapy. The choice of treatment depends on several factors, including the patient's overall health, the subtype of breast cancer, and the presence of other metastases.
Can breast cancer brain metastases be prevented?
+While there are no guaranteed methods to prevent BCBM, early detection and treatment of the primary breast cancer, as well as regular follow-up care, can reduce the risk of developing brain metastases. Ongoing research into the prevention and early detection of BCBM is critical for improving patient outcomes.
The stories of Sarah, Maria, and Emily, along with countless others, underscore the complexity and personal nature of breast cancer brain metastases. Each journey is unique, marked by challenges, resilience, and hope. As medical science continues to evolve, there is an increasing emphasis on personalized medicine, where treatments are tailored to the individual characteristics of each patient’s cancer. This personalized approach, combined with comprehensive support and ongoing research, holds the key to improving the lives of those affected by BCBM.

