Gi Bleed Diagnosis Code

Gastrointestinal (GI) bleeding is a serious medical condition that requires prompt diagnosis and treatment. The diagnosis of GI bleeding involves a combination of clinical evaluation, laboratory tests, and imaging studies. In the medical field, diagnosis codes are used to classify and code diseases, symptoms, and procedures. For GI bleeding, the diagnosis code depends on the location, severity, and cause of the bleeding.
The International Classification of Diseases, Tenth Revision (ICD-10), is a widely used system for coding diseases and health problems. According to the ICD-10, the diagnosis codes for GI bleeding are as follows:
- K92.0: Gastrointestinal hemorrhage, unspecified
- K92.1: Gastric hemorrhage
- K92.2: Duodenal hemorrhage
- K92.3: Hemorrhage of jejunum
- K92.4: Hemorrhage of ileum
- K92.5: Hemorrhage of colon
- K92.6: Hemorrhage of rectum
- K92.8: Other gastrointestinal hemorrhage
- K92.9: Gastrointestinal hemorrhage, unspecified
These codes are used to classify the diagnosis of GI bleeding based on the location of the bleeding. However, it’s essential to note that the diagnosis code may vary depending on the specific clinical scenario and the underlying cause of the bleeding.
In addition to the ICD-10 codes, other diagnosis codes may be used to classify GI bleeding, such as the Current Procedural Terminology (CPT) codes, which are used to code medical procedures. For example, the CPT code for upper GI endoscopy, which is a common procedure used to diagnose and treat GI bleeding, is 43235.
It’s also worth noting that the diagnosis of GI bleeding often involves a combination of clinical evaluation, laboratory tests, and imaging studies. The clinical evaluation includes a thorough medical history, physical examination, and vital sign assessment. Laboratory tests, such as complete blood count (CBC), blood urea nitrogen (BUN), and creatinine, are used to assess the severity of the bleeding and the patient’s overall health status. Imaging studies, such as computed tomography (CT) scan or magnetic resonance imaging (MRI), may be used to visualize the source of the bleeding and guide treatment.
In conclusion, the diagnosis code for GI bleeding depends on the location, severity, and cause of the bleeding. The ICD-10 codes are widely used to classify the diagnosis of GI bleeding, but other diagnosis codes, such as CPT codes, may also be used to code medical procedures. A thorough clinical evaluation, laboratory tests, and imaging studies are essential for accurate diagnosis and treatment of GI bleeding.
It's crucial to note that GI bleeding can be a life-threatening condition, and prompt medical attention is essential. If you or someone you know is experiencing symptoms of GI bleeding, such as vomiting blood, black tarry stools, or abdominal pain, seek medical help immediately.
Causes of GI Bleeding
GI bleeding can be caused by a variety of factors, including:
- Pepptic ulcers
- Gastroesophageal reflux disease (GERD)
- Helicobacter pylori infection
- Inflammatory bowel disease (IBD)
- Diverticulitis
- Colon cancer
- Angiodysplasia
- Vascular ectasias
Each of these conditions can cause GI bleeding, and the diagnosis and treatment will depend on the underlying cause.
Diagnosis of GI Bleeding
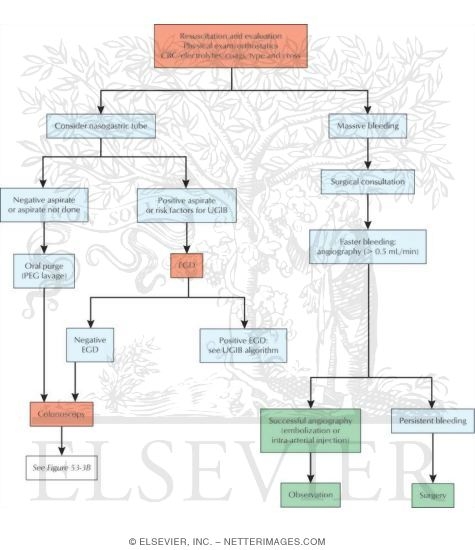
The diagnosis of GI bleeding involves a combination of clinical evaluation, laboratory tests, and imaging studies. The clinical evaluation includes a thorough medical history, physical examination, and vital sign assessment. Laboratory tests, such as CBC, BUN, and creatinine, are used to assess the severity of the bleeding and the patient’s overall health status. Imaging studies, such as CT scan or MRI, may be used to visualize the source of the bleeding and guide treatment.
Step-by-Step Approach to Diagnosing GI Bleeding
- Take a thorough medical history to identify risk factors and previous episodes of GI bleeding
- Perform a physical examination to assess vital signs and abdominal tenderness
- Order laboratory tests, such as CBC, BUN, and creatinine, to assess the severity of the bleeding and the patient's overall health status
- Perform imaging studies, such as CT scan or MRI, to visualize the source of the bleeding and guide treatment
- Consider upper GI endoscopy or colonoscopy to visualize the upper or lower GI tract and diagnose the cause of the bleeding
Treatment of GI Bleeding
The treatment of GI bleeding depends on the location, severity, and cause of the bleeding. Treatment options may include:
- Endoscopy to visualize the source of the bleeding and apply treatment, such as cauterization or clipping
- Medications, such as proton pump inhibitors or H2 blockers, to reduce acid production and promote healing
- Transfusions to replace lost blood and stabilize the patient
- Surgery to repair or remove the source of the bleeding
It’s essential to note that the treatment of GI bleeding should be individualized based on the patient’s specific needs and medical history.
Pros and Cons of Different Treatment Options for GI Bleeding
| Treatment Option | Pros | Cons |
|---|---|---|
| Endoscopy | Minimally invasive, high success rate, can diagnose and treat the cause of the bleeding | Risk of perforation, bleeding, or infection |
| Medications | Non-invasive, can reduce acid production and promote healing | |
| Transfusions | Can replace lost blood and stabilize the patient | Risk of transfusion reactions, can be expensive |
| Surgery | Can repair or remove the source of the bleeding | Risk of complications, can be invasive and expensive |
FAQ Section
What are the symptoms of GI bleeding?
+The symptoms of GI bleeding may include vomiting blood, black tarry stools, abdominal pain, and weakness or fatigue.
How is GI bleeding diagnosed?
+GI bleeding is diagnosed using a combination of clinical evaluation, laboratory tests, and imaging studies, such as upper GI endoscopy or colonoscopy.
What are the treatment options for GI bleeding?
+The treatment options for GI bleeding include endoscopy, medications, transfusions, and surgery, depending on the location, severity, and cause of the bleeding.
Can GI bleeding be prevented?
+Some cases of GI bleeding can be prevented by avoiding certain medications, such as nonsteroidal anti-inflammatory drugs (NSAIDs), and managing underlying medical conditions, such as GERD or IBD.
What is the prognosis for GI bleeding?
+The prognosis for GI bleeding depends on the location, severity, and cause of the bleeding, as well as the patient's overall health status. With prompt medical attention, the prognosis is generally good, but severe cases can be life-threatening.
In conclusion, GI bleeding is a serious medical condition that requires prompt diagnosis and treatment. The diagnosis of GI bleeding involves a combination of clinical evaluation, laboratory tests, and imaging studies. Treatment options depend on the location, severity, and cause of the bleeding, and may include endoscopy, medications, transfusions, and surgery. By understanding the causes, symptoms, diagnosis, and treatment options for GI bleeding, patients and healthcare providers can work together to prevent and manage this condition.



