Newborn Coombs Test: Results And Treatment Explained
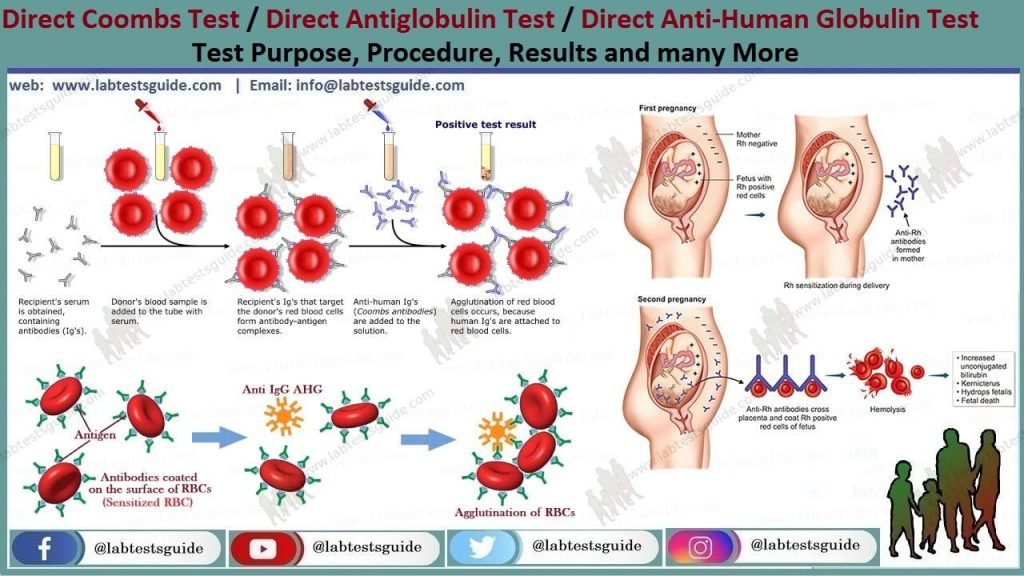
The newborn Coombs test, also known as the direct Coombs test or direct antiglobulin test, is a medical procedure performed on newborn babies to detect the presence of antibodies or complement proteins that are attached to the surface of their red blood cells. This test is crucial in identifying hemolytic disease of the newborn, a condition that occurs when the mother’s immune system produces antibodies against the baby’s red blood cells, leading to their destruction.
Why is the Newborn Coombs Test Performed?
The newborn Coombs test is typically performed when a mother has a history of producing antibodies against her baby’s red blood cells, a condition known as isoimmunization. This can occur when the mother’s blood type is Rh-negative and the baby’s blood type is Rh-positive, or when the mother has been sensitized to other red blood cell antigens during a previous pregnancy or blood transfusion. The test is also performed on babies who exhibit symptoms of hemolytic disease, such as jaundice, anemia, or hepatosplenomegaly.
How is the Newborn Coombs Test Performed?
The newborn Coombs test involves collecting a sample of the baby’s blood, typically from a heel prick or venipuncture. The blood sample is then sent to a laboratory where it is mixed with special reagents that react with the antibodies or complement proteins attached to the surface of the red blood cells. If the test is positive, it indicates that the baby’s red blood cells are coated with antibodies or complement proteins, which can lead to their destruction.
Understanding the Results of the Newborn Coombs Test
The results of the newborn Coombs test can be either positive or negative. A positive result indicates that the baby’s red blood cells are sensitized, meaning that they have antibodies or complement proteins attached to their surface. The severity of the result can vary, ranging from a weakly positive result, which may not require treatment, to a strongly positive result, which can indicate severe hemolytic disease.
A negative result, on the other hand, indicates that the baby’s red blood cells are not sensitized, and the risk of hemolytic disease is low. However, a negative result does not completely rule out the possibility of hemolytic disease, as some cases may not be detected by the Coombs test.
Treatment Options for a Positive Newborn Coombs Test Result
If the newborn Coombs test result is positive, treatment options will depend on the severity of the result and the presence of symptoms. In some cases, no treatment may be necessary, and the baby may simply be monitored for signs of hemolytic disease. In more severe cases, treatment options may include:
- Phototherapy: This involves exposing the baby to special lights that help break down bilirubin, a byproduct of red blood cell destruction that can cause jaundice.
- Exchange transfusion: This involves replacing the baby’s blood with donor blood to remove the sensitized red blood cells and reduce the risk of hemolytic disease.
- Intravenous immunoglobulin (IVIG): This involves administering antibodies that can help reduce the severity of hemolytic disease.
In some cases, treatment may also involve monitoring the baby’s bilirubin levels, complete blood count, and liver function to ensure that the condition is not worsening.
Complications and Risks Associated with the Newborn Coombs Test
While the newborn Coombs test is generally a safe procedure, there are some complications and risks associated with it. These may include:
- False positive results: In some cases, the test may produce a false positive result, which can lead to unnecessary treatment and stress for the parents.
- False negative results: Conversely, the test may produce a false negative result, which can lead to delayed diagnosis and treatment of hemolytic disease.
- Blood sample collection risks: The process of collecting a blood sample from the baby can carry risks, such as bleeding, infection, or bruising.
FAQs About the Newborn Coombs Test
What is the purpose of the newborn Coombs test?
+The newborn Coombs test is performed to detect the presence of antibodies or complement proteins attached to the surface of a newborn baby's red blood cells, which can indicate hemolytic disease of the newborn.
What are the risks associated with the newborn Coombs test?
+The risks associated with the newborn Coombs test include false positive or false negative results, bleeding, infection, or bruising during blood sample collection.
How is the newborn Coombs test performed?
+The newborn Coombs test involves collecting a blood sample from the baby, which is then sent to a laboratory for analysis.
What are the treatment options for a positive newborn Coombs test result?
+Treatment options for a positive newborn Coombs test result may include phototherapy, exchange transfusion, or intravenous immunoglobulin (IVIG), depending on the severity of the result and the presence of symptoms.
In conclusion, the newborn Coombs test is an essential medical procedure that helps detect the presence of antibodies or complement proteins attached to the surface of a newborn baby’s red blood cells, indicating hemolytic disease of the newborn. While the test is generally safe, there are some complications and risks associated with it, and treatment options will depend on the severity of the result and the presence of symptoms. By understanding the purpose, risks, and treatment options associated with the newborn Coombs test, parents can make informed decisions about their baby’s care and ensure the best possible outcome.