Posterior Spinal Fusion With Instrumentation
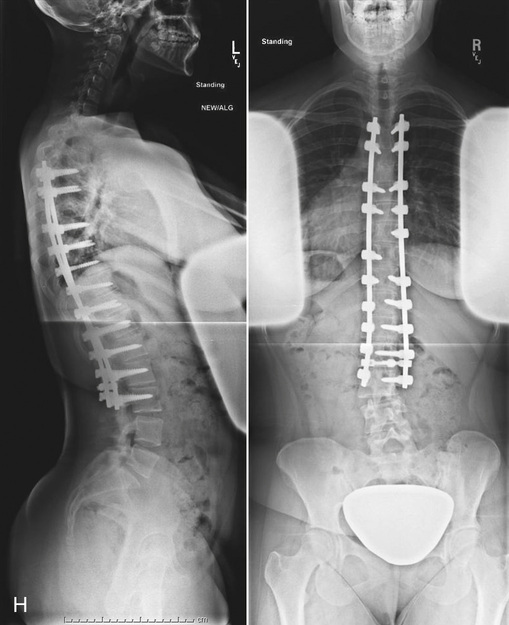
Posterior spinal fusion with instrumentation is a surgical procedure designed to stabilize and fuse two or more vertebrae together, using a combination of bone grafts and internal fixation devices. This approach is often employed to treat a variety of spinal conditions, including degenerative disc disease, spondylolisthesis, spinal fractures, and spinal deformities such as scoliosis or kyphosis.
Overview of the Procedure
The procedure typically begins with the patient being placed under general anesthesia and positioned prone on a specially designed operating table. The surgeon then makes an incision in the midline of the back, extending from the upper to the lower levels of the spine to be fused. The muscles are carefully dissected and retracted to expose the posterior elements of the spine, including the spinous processes, laminae, and transverse processes.
Once the spine is exposed, the surgeon prepares the vertebrae to be fused by removing any damaged or diseased disc material, bone spurs, or other tissues that may be causing compression on the spinal cord or nerves. The bone grafts, which may be taken from the patient’s own body (autograft) or from a donor (allograft), are then carefully placed between the vertebrae to promote fusion.
Instrumentation in Posterior Spinal Fusion
Instrumentation plays a critical role in posterior spinal fusion, as it provides immediate stability to the spine, allowing for early mobilization and rehabilitation. The most common types of instrumentation used in posterior spinal fusion include:
- Pedicle Screws: These are the most commonly used type of instrumentation. They are inserted into the pedicles of the vertebrae, which are the strong posterior elements of the vertebra that connect the posterior arch to the vertebral body. The screws are then connected by rods or plates that run along the length of the spine to be fused.
- Hooks: These are less commonly used now but can be attached to the laminae or transverse processes of the vertebrae. They are connected by rods to provide stability.
- Sublaminar Wires or Cables: These are placed under the laminae of the vertebrae and are usually used in conjunction with hooks and rods.
The choice of instrumentation depends on several factors, including the specific spinal condition being treated, the level and extent of the fusion, the quality of the patient’s bone, and the surgeon’s preference.
Benefits and Risks
Posterior spinal fusion with instrumentation offers several benefits, including:
- Stabilization of the Spine: Immediate stability is provided, which can lead to quicker recovery and less risk of complications.
- Promotion of Fusion: The instrumentation helps to maintain the vertebrae in the correct position, promoting successful fusion.
- Relief of Symptoms: By stabilizing the spine and promoting fusion, the procedure can help alleviate pain, numbness, tingling, and muscle weakness caused by spinal instability or compression of the spinal cord or nerves.
However, as with any surgical procedure, posterior spinal fusion with instrumentation also carries risks and potential complications, including:
- Infection
- Bleeding or Hematoma
- Nerve Damage
- Instrumentation Failure
- Pseudarthrosis (Failure of Fusion)
- Adjacent Segment Disease
Recovery and Rehabilitation
The recovery process after posterior spinal fusion with instrumentation can be lengthy, typically taking several months to a year or more for full recovery. Immediately after surgery, patients usually spend a few days in the hospital for pain management and monitoring. Once discharged, patients are advised to avoid heavy lifting, bending, and twisting, and to follow a specific rehabilitation program that may include physical therapy to improve mobility and strength.
Conclusion
Posterior spinal fusion with instrumentation is a complex surgical procedure that requires careful consideration and planning. While it offers significant benefits for patients with certain spinal conditions, it also carries potential risks and complications. Advances in surgical techniques and instrumentation continue to improve outcomes, making this procedure a viable treatment option for many patients seeking relief from spinal disorders.
What are the most common indications for posterior spinal fusion with instrumentation?
+Posterior spinal fusion with instrumentation is commonly indicated for conditions such as degenerative disc disease, spondylolisthesis, spinal fractures, and spinal deformities like scoliosis or kyphosis.
How long does it take to recover from posterior spinal fusion surgery?
+Recovery from posterior spinal fusion surgery can take several months to a year or more. The initial period involves pain management and monitoring, followed by a gradual return to normal activities under the guidance of a rehabilitation program.
What are the potential risks and complications of posterior spinal fusion with instrumentation?
+Potential risks and complications include infection, bleeding, nerve damage, instrumentation failure, pseudarthrosis (failure of fusion), and adjacent segment disease. It's crucial to discuss these risks with a healthcare provider before undergoing the procedure.
In the realm of spinal surgery, posterior spinal fusion with instrumentation stands as a testament to the evolving capabilities of medical science, offering hope and relief to countless individuals affected by spinal disorders. Through continued advancements in surgical techniques and technology, the outlook for patients undergoing this procedure continues to improve, highlighting the importance of staying informed and seeking professional advice when considering treatment options.

